Booking Health Unveils New Study: Role of Immunotherapy in Extending Life Expectancy for Stage4 Cervical Cancer Patients
Langenfeld, Germany, Aug. 11, 2025 (GLOBE NEWSWIRE) -- Booking Health, a global leader in medical treatment coordination, today unveiled a new study titled Role of Immunotherapy in Extending Life Expectancy for Stage 4 Cervical Cancer Patients. The report outlines how cutting-edge immunotherapy is reshaping care for women with advanced cervical cancer, offering new pathways to longer survival and improved quality of life, particularly in cases resistant to standard treatments.
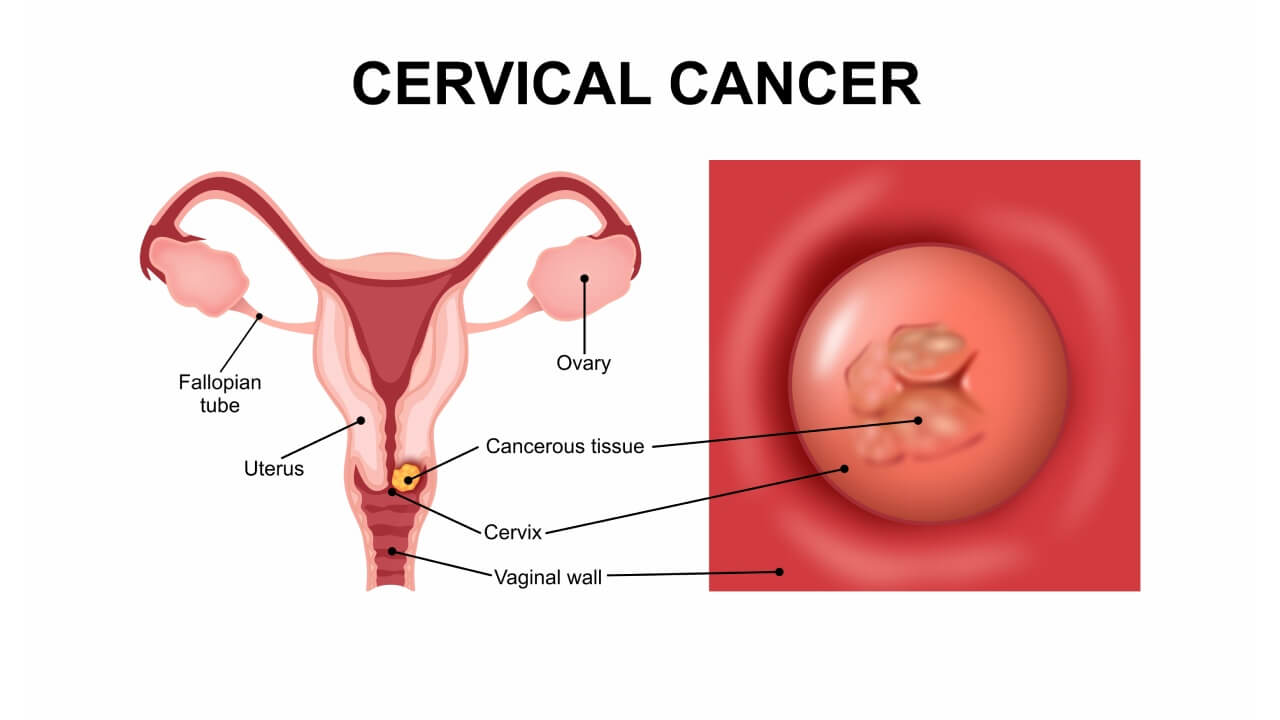
Cervical Cancer
Immunotherapy is redefining how doctors treat women diagnosed with stage 4 cervical cancer – offering hope where traditional treatments often fall short. According to global cancer statistics provided by the World Health Organization, cervical cancer is still ranking as the fourth most frequently diagnosed cancer among women worldwide, with over 350,000 deaths reported in 2022 alone. Therefore, the need for more effective therapies is urgent.
Chemotherapy and radiation therapy remain standard for locally advanced and metastatic cervical cancer. However, they often come with harsh side effects and limited long-term benefit – especially in recurrent or PD-L1-positive cases. This is where immunotherapy is beginning to transform the way we treat cervical cancer.
By training the immune system to recognize and destroy cancer cells, this innovative approach is extending survival, improving quality of life, and reshaping the future of gynecologic oncology, according to the American Cancer Society. Leading the way in connecting patients with advanced treatment abroad is Booking Health, a global medical coordination platform that offers access to advanced cervical cancer treatment in the best European clinics.
Why Is Stage 4 Cervical Cancer So Hard to Treat?
Stage 4 cervical cancer is difficult to treat because it involves metastatic disease, where cancer has spread beyond the pelvis to distant organs, making it less responsive to traditional therapies such as chemotherapy and radiation. In many cases, the disease becomes persistent or recurrent, with fewer effective treatment options available, as reported by the National Cancer Institute.
Types of Advanced Cervical Cancer
Understanding the different stages helps clarify why some cases are more complex than others:
| Term | Definition | Treatment Challenge |
| Locally advanced cervical cancer | Cancer has spread beyond the cervix to nearby tissues (e.g., vagina, parametria) but not to distant organs | Often treated with chemoradiation, but recurrence risk remains |
| Recurrent cervical cancer | Cancer returns after a period of remission | May resist previously used therapies and require new approaches |
| Metastatic cervical cancer | Cancer spreads to distant organs like lungs, liver, or bones | Hard to target; systemic therapies often have limited success |
Most Common Cervical Cancer Types
-
- Squamous cell carcinoma – accounts for 80-90% of cases; originates in the ectocervix
-
- Adenocarcinoma – about 10-20% of cases; arises from glandular cells in the endocervix
- Adenosquamous carcinoma – a rarer subtype with mixed features
As reported by Cancer Research UK, each type may behave differently in terms of spread, immune response, and treatment sensitivity.
Limitations of Traditional Treatments
Standard treatments for advanced cervical cancer include:
-
- Chemotherapy: Often platinum-based; effectiveness diminishes over time;
-
- Radiation therapy: Can control local disease but may not impact distant metastases;
- Systemic therapies: Cause significant side effects, with limited survival benefit in persistent cervical cancer.
Moreover, the American Cancer Society reports that patients with persistent or metastatic disease often experience poor outcomes, with 5-year survival rates below 20% in stage 4 cases.
As such, gynecologic oncology experts have increasingly turned to immunotherapy to improve response rates and extend survival.
What Is Immunotherapy and How Does It Work for Cervical Cancer?
Immunotherapy for cervical cancer stimulates the body's own immune system to recognize and destroy cancer cells by targeting specific immune pathways. This approach is especially useful for patients with PD-L1–positive, recurrent, or metastatic cervical cancer who may not respond well to conventional treatments.
| Approach | Description | Relevance to Cervical Cancer |
| Immune checkpoint inhibitors | Block proteins (PD-1, PD-L1) that prevent immune cells from attacking cancer | Reactivates exhausted T cells to fight cervical cancer cells |
| Monoclonal antibodies | Lab-made antibodies designed to target specific tumor markers | Some bind PD-L1 or deliver cytotoxic agents directly to tumor cells |
| Cancer vaccines | Stimulate immune response to HPV or tumor-associated antigens | Promote lasting T cell activation and memory |
| Adoptive T cell therapy | Infuse engineered T cells that can attack tumor cells | Under investigation for recurrent cervical cancer |
The PD-1/PD-L1 Pathway
-
- PD-1 is a receptor on T cells that regulates immune response
-
- PD-L1 is often overexpressed on cervical cancer cells
-
- When PD-L1 binds to PD-1, it "switches off" the immune attack
- Checkpoint inhibitors block this interaction – reactivating T cells to destroy cancer cells
Why It Matters
-
- Many cervical tumors exhibit high PD-L1 expression, making them ideal candidates for immunotherapy.
-
- Successful treatment leads to greater T cell infiltration into tumors, enhancing immune surveillance.
- Patients often experience improved immune response and more durable control of the disease than with chemotherapy alone.
This therapeutic shift reflects a broader move toward personalized medicine in gynecologic oncology, targeting tumor-infiltrating lymphocytes and immune checkpoints rather than relying solely on cytotoxic drugs.
Findings from the Latest Clinical Trials
Recent phase III clinical trials have shown that combining immunotherapy with standard chemotherapy – or using it as a second-line option – can significantly extend survival and delay disease progression in patients with recurrent or metastatic cervical cancer.
These studies demonstrate that there has occurred a major shift in how advanced cervical cancer is treated, providing hope to patients who previously had limited options after conventional therapies failed.
Highlights from the Trials
-
- Patients receiving immunotherapy lived significantly longer than those on chemotherapy alone.
-
- Survival benefit was observed regardless of PD-L1 status, especially in recurrent cases after platinum-based treatment.
-
- Delays in disease progression gave patients more time with better quality of life.
- Immune checkpoint inhibitors helped reactivate the immune system's ability to target and destroy cervical cancer cells.
| Clinical Trial | Treatment Type | Median Overall Survival (OS) | Disease Control Outcome | Notes |
| Phase III Study | Immunotherapy + Chemo | Up to 28.6 months vs 16.5 months | Longer survival in all groups | Strongest benefit in PD-L1+ patients |
| Randomized Phase III Trial | Immunotherapy (2nd-line) | 11.7 months vs 8.5 months | Benefit seen in all PD-L1 levels | Works even after chemo failure |
* Both studies confirmed survival advantages without significantly higher severe side effects compared to chemotherapy alone.
What This Means for Patients
For women with recurrent, persistent, or metastatic cervical cancer, these results signal a new standard of care. Immunotherapy is not only more targeted than traditional therapies but also better tolerated, offering:
-
- A longer window of disease control (median progression-free survival extended);
-
- Improved quality of life with fewer systemic side effects;
- Hope for those who did not respond to chemotherapy or radiation.
This also opens the door for future therapies involving antibody drug conjugates, personalized immune profiling, and combination treatments that utilize both the immune system and conventional medicine. Today, cervical cancer cohorts worldwide are benefiting from a more individualized, immune-driven approach that redefines what is possible after recurrence or metastasis.
Who Benefits Most from Immunotherapy in Cervical Cancer?
Immunotherapy is most effective for patients with PD-L1-positive, recurrent, or metastatic cervical cancer, particularly when standard treatments like chemotherapy or radiation therapy have failed, as previously mentioned. These patients often have limited options, and immunotherapy provides a targeted approach that can activate the immune system to attack tumor cells more effectively.
Common Eligibility Criteria for Immunotherapy
Patients who may benefit from immunotherapy typically meet one or more of the following criteria:
-
- PD-L1 expression ≥1% (as determined by tumor biopsy);
-
- Recurrent or metastatic cervical cancer following standard treatment;
-
- Persistent squamous cell carcinoma that does not respond to initial therapies;
-
- Evidence of T cell infiltration or active immune cell presence within the tumor;
- No contraindications for immune checkpoint blockade (e.g., autoimmune diseases).
| Histology Type | Prevalence | Response to Immunotherapy |
| Squamous Cell Carcinoma | ~80-90% | Better overall immune response; more PD-L1 expression; strong T cell infiltration |
| Adenocarcinoma | ~10-20% | Slightly lower PD-L1 expression; emerging data still promising |
| Adenosquamous/Mixed | <5% | Limited clinical data; under investigation |
While both subtypes may benefit, squamous cell carcinoma tends to respond more favorably due to its immunogenicity and higher prevalence of immune markers like PD-L1.
Why This Is Important
Understanding which patients are most likely to respond helps oncologists personalize therapy, avoid unnecessary toxicity, and improve overall outcomes in metastatic cervical cancer patients. As clinical trials continue to evolve, biomarkers like PD-L1, tumor-infiltrating lymphocytes, and even genomic profiling are playing a larger role in guiding treatment selection.
What Are the Current Limitations and Side Effects of Immunotherapy?
While immunotherapy is an innovative option in cervical cancer treatment, it is not without limitations. Not all patients experience a positive immune response, and treatment can lead to side effects caused by overstimulation of the immune system.
Main Limitations of Immunotherapy for Cervical Cancer
-
- Variable response rates: Only patients with specific tumor profiles (e.g., PD-L1-positive tumors or high T cell infiltration) tend to respond.
-
- Delayed response: Unlike chemotherapy, benefits may take weeks or months to appear.
-
- Immune hyperactivation: Some patients may develop autoimmune-like reactions when the immune system attacks healthy tissue.
-
- High costs: Immunotherapy is expensive, and coverage varies widely by country and provider.
- Limited access: Not all regions offer advanced immune-based therapies or diagnostic testing.
| Side Effect Type | Description | Frequency |
| Colitis | Inflammation of the colon causing diarrhea | Moderate |
| Thyroiditis/Hypothyroidism | Immune attack on the thyroid | Common |
| Dermatitis or skin rash | Immune-related skin inflammation | Common |
| Fatigue and joint pain | General inflammatory response | Mild to moderate |
| Pneumonitis | Lung inflammation (rare but serious) | Rare |
Cleveland Clinic highlights that these side effects are often immune-related and differ from those of chemotherapy, which typically causes nausea, hair loss, and bone marrow suppression. Most immune-related reactions are manageable with corticosteroids or immunosuppressive agents when diagnosed early.
Importance of Tumor Profiling and Biomarker Testing
Before initiating immunotherapy, tumor profiling is crucial. Tests that assess PD-L1 expression, tumor mutational burden, and immune cell markers help determine whether a patient is a good candidate. This ensures that patients treated are those most likely to benefit from therapy while minimizing unnecessary risks.
Why Are More Patients Going Abroad for Cervical Cancer Immunotherapy?
Many cervical cancer patients choose to go abroad for immunotherapy because of faster access, broader treatment options, and advanced clinical expertise – especially in countries known for innovation in gynecologic oncology. In many parts of the world, patients face long wait times, outdated systemic therapies, or limited access to next-generation immune system-based treatments.
This is especially critical for women with advanced or recurrent cervical cancer, where timely intervention can directly affect survival and quality of life. In contrast, specialized cancer centers in countries like Germany offer accelerated treatment pathways, advanced diagnostics, and access to experimental options not yet widely available elsewhere.
Primary Reasons Patients Travel Abroad for Treatment
-
- Limited access at home: In some countries, immune checkpoint inhibitors and personalized immunotherapy are not yet standard care – or are cost-prohibitive without insurance support.
- Delays in diagnosis or therapy: Long waitlists for oncology consultations or biopsy testing can result in treatment delays that worsen outcomes.
Patients who choose to treat cervical cancer abroad often report improved outcomes, better coordination, and more comprehensive care – especially when guided by experienced facilitators like Booking Health.
From Research to Results: How Immunotherapy Extends Life Expectancy
Recent clinical advances highlight the growing role of immunotherapy in improving life expectancy for patients with stage 4 cervical cancer. Immune checkpoint inhibitors and other immune-based treatments are showing encouraging results, particularly for recurrent, metastatic, and PD‑L1‑positive cervical cancers, where traditional chemotherapy offers limited benefit. By stimulating the body’s own immune system to recognize and attack tumor cells, these therapies have been linked to longer survival and improved progression-free outcomes in international studies.
Access to such innovative care remains uneven, prompting patients to seek specialized oncology centers abroad. Through coordination platforms such as Booking Health, individuals are able to connect with leading hospitals in Germany and other countries that offer advanced cervical cancer immunotherapy programs. These multidisciplinary approaches combine personalized treatment planning, modern diagnostics, and targeted immune modulation to address late‑stage disease. As immunotherapy research continues to expand, it represents a significant shift in the management of advanced cervical cancer, giving more women a realistic chance at extended survival and an improved quality of life.
Key Takeaways: Immunotherapy's Impact on Advanced Cervical Cancer
-
- Immunotherapy offers hope for women with stage 4 cervical cancer, especially when other treatments have failed.
-
- It works by strengthening the immune system to recognize and eliminate cancer cells more effectively.
-
- Most effective in patients with PD-L1-positive, recurrent, metastatic, or invasive cervical cancer.
-
- Recent phase III clinical trials show longer survival and improved median progression-free survival compared to chemotherapy alone.
- Booking Health connects international patients with leading European hospitals that specialize in cervical cancer immunotherapy and personalized care.
These breakthroughs represent a major advancement in the treatment of metastatic cervical cancer – delivering not only longer survival, but also a significantly improved quality of life. To explore your personalized treatment options, contact Booking Health today and take the next step toward advanced cervical cancer care.
Side_Effects
About Booking Health
Booking Health™ is the international platform for rapid access to innovative treatments in the world’s leading certified clinics. Our network features over 250 top-tier hospitals across the globe, all distinguished by the exceptional levels of medical accreditation and expertise. By arranging care with the help of Booking Health company, you benefit from comprehensive medical support based on the latest innovations and personalized coordination. We offer cost saving up to 70% compared to direct booking via clinics — all without compromising on quality. Choosing Booking Health means more than just acquiring access to innovative world-class therapy - it means saving valuable time knowing that every detail is handled by professionals. Headquartered in Bad Hönningen, Germany and officially registered in Düsseldorf under HRB 106466, Booking Health proudly consults patients from over 75 countries for over a decade, offering services in 11 languages.
Press inquiries
Booking Health
https://bookinghealth.com/
Lena Hanten
marketing@bookinghealth.com

Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.

